The original article was provided by Abena.
Obesity is a significant factor in the development of incontinence, impacting both physical and emotional well-being. Globally, 13% of adults are obese, with obesity rates nearly tripling since 1975. This article aims to simplify the link between obesity and incontinence and offers insights into everyday care.
What is Obesity?
Obesity results from an energy surplus—consuming more calories than needed. This imbalance, driven by factors like high-calorie diets and sedentary lifestyles, has led to a global obesity surge. Body mass index (BMI), a tool categorizing individuals based on height and weight, is crucial for understanding obesity's impact.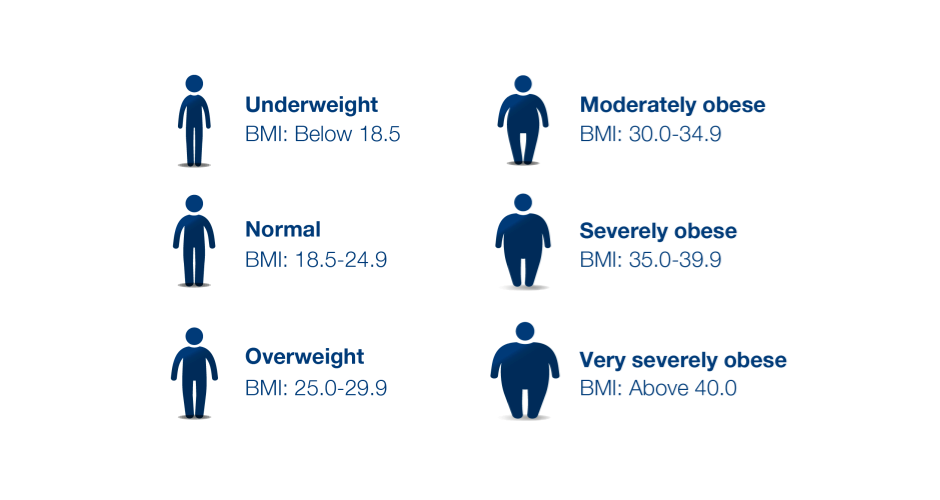
How are Obesity and Incontinence Linked?
Obesity increases intra-abdominal pressure, affecting the bladder and pelvic floor muscles. Research establishes a strong connection between obesity and urinary incontinence, particularly in women. Stress incontinence, linked to a BMI over 30, becomes more prevalent. Bariatric patients often face stress or urge incontinence, and sometimes a combination called mixed incontinence.
Working with Obese Patients
Understanding and addressing societal stigmas associated with obesity is vital when caring for patients. Negative beliefs can lead to delayed care-seeking, making it crucial to approach treatment with empathy. Additionally, skin issues, common in bariatric individuals, demand special attention. Skinfolds, prone to microorganism growth, require gentle cleansing, breathable protection, and proper moisture management.
Treatment Options
Weight loss, through a holistic approach, is a primary treatment for incontinence in overweight and obese individuals. Studies show that a 5-10% reduction in total body weight significantly alleviates urinary incontinence. However, addressing weight stigma is essential, as it affects individuals both physically and psychologically. Consulting with a doctor and dietitian before initiating a weight loss plan is crucial.
Obesity and Other Risk Factors
Beyond incontinence, obesity is associated with various health risks, including cardiovascular disease, type 2 diabetes, cancer, and more. Weight stigma further contributes to depression, suicidal ideation, and low self-esteem. Recognizing obesity's complexity and adopting a holistic approach to treatment is essential for overall well-being.
In conclusion, the intricate relationship between obesity and incontinence necessitates compassionate and tailored care. Prioritizing patient comfort, understanding the link between obesity and health complications, and combating weight stigma are integral to providing comprehensive healthcare for individuals living with obesity.
During the journey, you can always ask help to enhance the daily comfort and independence, to improve overall quality of life.
[SEEK ABENA BARIATRIC INCONTINENCE SOLUTIONS]

